by Ron Harrington
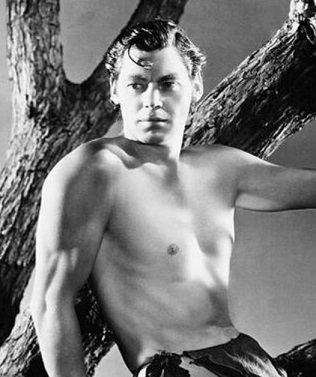
As a young lad growing up in the 60’s I spent many rainy Saturday afternoons watching old movies, some of which featured Tarzan, the Ape Man. I developed a great admiration for Tarzan, with his lean, strong physique and rude animal health, and I hoped to emulate his life as nearly as possible. (I was thwarted in this effort chiefly by a lack of suitable vines in the local trees and a debilitating fear of quicksand.) Though my desire to swing through the trees has waned considerably, I would still like a portion of Tarzan’s health and vitality—as would we all.
For we are a very un-Tarzan-like population. Recent reports on the health status of Americans are alarming. According to the CDC, over 35 million Americans have type II diabetes (and about 8 million of those don’t know they have it); almost 100 million Americans (including about half of those over 65) have prediabetes; three quarters of Americans are overweight or obese. And not all of those with diabetes or prediabetes are overweight—the lean can be afflicted as well. And it’s only getting worse.
Type II diabetes among children and adolescents has almost doubled in just the last twenty years. Almost twenty percent of children and adolescents have prediabetes, and one quarter of young adults have it. It is clear that America has a burgeoning crisis in metabolic health.
“Metabolic health” refers to how efficient our bodies are at breaking down the food we eat, getting it to the individual cells where it is needed, and producing the energy those cells need to function properly. It is foundational to every process in our bodies. When our metabolic processes become dysfunctional, our whole body suffers. Metabolic dysfunction leaves us feeling unwell, accelerates aging, and can contribute to the chronic diseases we all fear: diabetes, heart disease, cancer, Alzheimer’s, mental illness, and many others.
Some years ago I was in terrible metabolic health. Over the course of forty years I had managed to pack on an extra 120 pounds. And I felt horrible. My lab numbers from a recent physical were awful, and I knew I was headed for major problems if I didn’t make some big changes.
I had of course tried diets and exercise, and nothing much worked for long. I had been told that poor metabolic health was caused by being overweight, and the weight gain was caused by consuming more calories than I was expending. Being a curious fellow, I began to wonder why I was consuming more calories than I was expending. That curiosity led me to learn what elements of my diet and lifestyle led to metabolic dysfunction and what changes to make to recover from it. I learned that weight gain is just one of many possible unfortunate effects of metabolic dysfunction, and that weight loss is often one happy side effect of reversing it.
Me, 1982 (age 22):
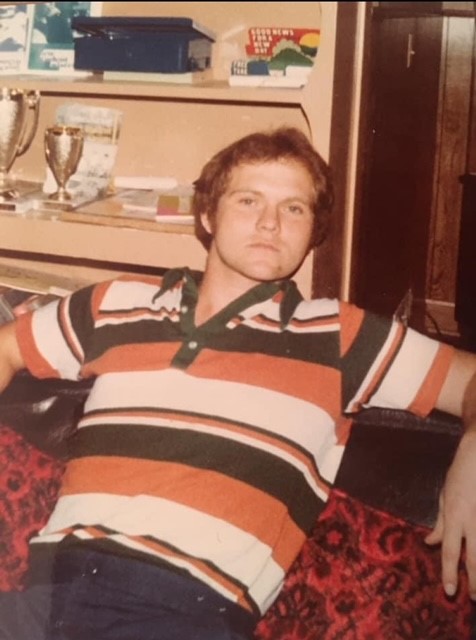
Me, 2020 (age 60):

Me, 2025 (age 65):

I’ve lost a considerable amount of weight, but more important, I have greatly improved my metabolic health. My lab numbers are no longer in the tank, and my energy level and mental clarity have much improved. I am as yet unlikely to get invited to hang out with Derek Zoolander, but I have made a lot of progress. I’ve been reliably informed by my children that I now resemble a Goron, some creature from the Zelda video games; I don’t know what a Goron looks like, but I can only assume they are a handsome, well-proportioned species.
[Editor’s note: This is a Goron:]

The purpose of this story is to share with you some of what I have learned along the way in hopes you might find something useful in it. I am not selling anything, nor am I pushing a particular diet—what we learn from this story can apply to a lot of different ways of eating, from vegan to carnivore.
Also, I am not going to tell you what you should eat or not eat. I will explain, as best I can, how our bodies process the different types of foods we eat, and the impact each has on our metabolic health, so that you can make informed choices about your own way of eating.
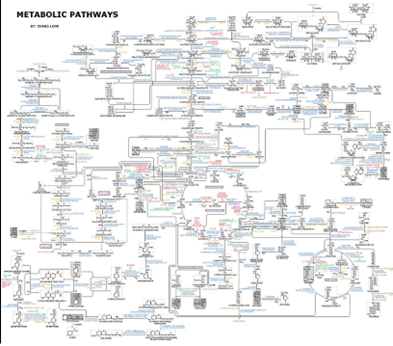
There are a couple of ways we could approach this discussion. One would be to fully explore this chart detailing our metabolic pathways:
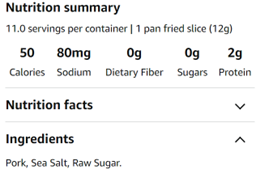
The other way would be to talk about Tarzan, the Ape Man:
I’m going with Tarzan.
To help us understand metabolism and how it can go wrong, I’m going to tell a part of Tarzan’s story that the original author curiously omitted: Tarzan’s metabolic processes. Even though everything that follows is grossly oversimplified, it will still be necessary to get a little further into the scientific weeds than some of us might like, so gird your loins. (As Albert Einstein supposedly said, “Everything should be as simple as possible, but no simpler.”)
Before I go on, I should point out that it would be madness for you to take what follows—the ravings of a random old man on the internet—at face value. You should do your own reading to figure out whether you think what I am saying is true. And I’m begging you, with tears in my eyes, don’t make any major changes to your diet or exercise routine without consulting a medical professional.
After the story you’ll find other posts explaining some of the science behind all this, some ideas about how someone might go about following Tarzan’s path back to metabolic health, and links to references.
Let us begin.
Tarzan in the Jungle
As Tarzan awoke from pleasant dreams he felt the sunlight on his face. He had fallen asleep in a clearing beside the fire where he and his friends from the village had spent a pleasant evening sharing stories. He cleared his throat and let loose with a few of his patented yells, just to let everyone know he was awake and on the job. He hopped into a tree, grabbed a vine, and made his rounds to check on his animal friends and the inhabitants of the nearby village. Assured that all was well and feeling a bit peckish, he set about to gather the makings of a good meal. He checked on a snare he had set up the evening before and found he had captured a nice, plump fowl. After gathering a few vegetables and some berries he built a fire to cook it all up. What is of particular interest to us in this story is what happens to the food that Tarzan eats. We know that various enzymes and chemicals in Tarzan’s digestive tract will break down the food into forms that his cells can make use of. But not all foods are dealt with in the same way.
Tarzan, like the rest of us, has about 37 trillion cells in his body, all of which require a constant supply of fuel, or they die. The fuel the cells need comes from the food Tarzan eats, and by the time it gets to the cells it has been broken down to the molecular level so it can be processed by the mitochondria in his cells. (Mitochondria are tiny structures in the cells that turn the food molecules into energy. They are known as the “powerhouse” of the cells.)

Mitochondrion (Artist’s rendering)
As Tarzan digested the meal his body dealt with the different nutrients, each in its own way. The fat in the meal mostly got sent to the fat cells for temporary storage so Tarzan could use it for fuel between meals. The protein was used to build and repair muscle and other things his cells needed to thrive. The starch in the veggies turned to glucose as it was digested. Since Tarzan’s body knew that high levels of glucose in his blood would wreak all sorts of havoc, his pancreas responded by releasing insulin to clean it up. The insulin told Tarzan’s fat cells to grab as much fat as they could and hold on to it so his other cells could focus on burning up the glucose. The insulin also told Tarzan’s liver to start converting excess glucose to fat. (I must pause here to point out that “Tarzan’s Liver” would be an excellent name for a rock band.) That fat was also sent on to the fat cells for storage. Some of the fructose in the berries (the kind of sugar that makes them sweet) was converted to glucose in his intestines; the rest got sent to his liver, where some of it was converted to glucose and stored in his liver and the rest converted to fat and forwarded on to his fat cells for storage. For a while after his meal, Tarzan’s cells were burning a lot of glucose.
But as the glucose levels in his blood dropped, so did the insulin. As the insulin dropped, the fat cells started releasing fat so it could be burned.
Between meals, Tarzan’s cells mostly burned fat.
Tarzan spent the afternoon doing Tarzan-like things—stopping a rampaging elephant from destroying a village here, rescuing a toddler from a crocodile there. He took his responsibilities as King of the Jungle seriously. As the day wore on, Tarzan’s fat reserves had been dropping, and something deep in his brain became alarmed. It didn’t want Tarzan’s fat reserves to fall too low— they may be needed one day if food gets scarce. It caused hormones to be released that made Tarzan to start to feel hungry.
As evening fell he encountered some friends from the village who were returning from a hunt. They had speared a nice fat boar and were planning a feast, which Tarzan was invited to join. They roasted the boar meat over an open fire and settled in to eat. Along with the boar, they had roasted some yams and had some berries they’d gathered for dessert.
As Tarzan ate the meal his body dealt with the nutrients as before. The fat he ate was sent to fat cells for storage. Some of the fructose was converted to glucose, and the rest went to his liver where it was converted to glucose and stored and the rest converted to fat, which was then sent to the fat cells for storage. The starch in the meal was broken down into glucose, which caused his insulin levels to rise. The insulin told Tarzan’s fat cells to grab fat and hold on to it, his muscles to burn glucose for fuel, and his liver to convert glucose to fat.
Since swinging on vines, running down elephants, and wrestling crocodiles had put a lot of stress on Tarzan’s muscles and his heart and lungs, his body responded by releasing hormones that triggered growth and repair, to ensure he would be prepared should such things happen again. The protein from the meal was used to repair and build muscle and other tissues.
After the meal Tarzan sat by the fire with his friends, telling stories and relaxing. As the sun set, hormones were released that started preparing Tarzan for sleep. He watched the fire until he drifted off.
Meanwhile, as his glucose levels dropped his insulin followed suit. As the insulin dropped, fat started to flow out of his fat cells to be used for fuel as he slept. During the night Tarzan’s liver released some of the stored glucose to keep the levels in his blood stable.
That pattern repeated, day by day. He would eat a meal, glucose was burned with some converted to fat, fat was stored away until the glucose in Tarzan’s blood reached a safe level, and then the fat flowed out of his fat cells and was burned for energy until his next meal. His mitochondria were beavering away, turning the nutrients into the energy his cells needed. He was an active man, and that energy was being burned. His mitochondria were content. A complex interplay of hormones worked to ensure that he was taking in the same amount of energy he was burning. He didn’t have to count the calories he was eating, or track his activity to make sure he was active enough to burn off those calories. His hormones took care of that.
And so Tarzan’s life went–and would likely have gone on for a long time had not something unexpected happened: Jane.
Jane Porter was an American woman among a group of travelers who were marooned by a shipwreck on the coast near Tarzan’s home. Tarzan found her lovely and was determined to share his life with her. The details of their relationship and how Jane was ultimately rescued need not detain us, except to say that Jane ended up back in America, and Tarzan followed her there.
Tarzan in America
As Tarzan awoke from uneasy dreams he heard the sound of a jet airplane rattling the windows of his motel room. His flight to America had arrived late and he had checked into the first motel he found near the airport. Feeling hungry, he made his way down to the motel restaurant. After observing what a diner at a nearby table was eating, he asked for the same: eggs with bacon, hash browns, and a stack of pancakes. His metabolic system was entirely unprepared for what was about to happen.
As he consumed the meal and began to digest it, his body went to work metabolizing the meal. The fat in the meal was broken down and sent to the fat cells for storage, as usual. The protein was used for growth and repair.
The sugar in the syrup and the pancakes was split into fructose and glucose. Some of the fructose was converted to glucose, with the rest sent to Tarzan’s liver to be processed. There it was mostly converted to fat and sent to his fat cells for storage. Tarzan’s liver was overwhelmed. While it could easily handle the fructose in a serving of berries, it could not keep up with such an onslaught. Some of the fructose ended up being deposited as fat in his liver.
The starch in the hash browns and pancakes—and there was a lot of starch— was immediately converted into glucose. That glucose, along with the glucose from the sugar, sent Tarzan’s pancreas into panic mode. (“Tarzan’s Pancreas” would not be a particularly good name for a rock band.) They had never seen such a load of glucose. As Tarzan’s blood glucose levels rose, his levels of insulin rose with it.
The insulin told the fat cells to start taking in fat and to hold onto it. It told the muscles and other tissues to burn glucose. It told his liver to convert all that excess glucose into fat, a process that Tarzan’s liver struggled to accomplish. Some of the fat ended up stored locally in his liver.
It took a good deal longer for Tarzan’s insulin to drop low enough for his brain to get the signal that he had plenty of fat stored up, so his brain became concerned that he might be starving. The insulin kept the fat locked up in his fat cells so he couldn’t use it for energy. He felt strangely sluggish and was thinking of food throughout the morning, even though he was stuffed.
Upon arrival in America Tarzan was in need of a job so he could support himself as he courted Jane. He quickly found one at a call center doing technical support for a software company. (And if you think his utter lack of technical knowledge would have made him an unlikely candidate for a job in technical support, then you haven’t called many technical support lines.)
On the way to work his first day Tarzan stopped by Starbucks, as was the local custom, and selected a Café Mocha with Whipped Cream and a Cheese Danish.
The fat in the meal was sent to the fat cells for storage. The small amount of protein in the meal was used for growth and repair. The added sugar was split into fructose and glucose. Some of the fructose was converted to glucose, with the rest sent to Tarzan’s liver where most was converted into fat and sent to the fat cells for storage. It was a much higher load of fructose than Tarzan’s liver was designed to handle, and so some fat ended up deposited locally in his liver. The starch in the Danish was converted to glucose, which, along with the glucose in the table sugar, prompted the pancreas to release insulin. It told the fat cells to grab fat and hold onto it, the muscles to burn glucose, and the liver to convert glucose to fat. It was a much higher glucose load than Tarzan’s liver was designed to handle, and some of the fat ended up being deposited locally in the liver.
Once again Tarzan’s insulin spike went higher and lasted longer than it ever did back in the jungle. It took longer for his brain to get the signal that his fat reserves were adequate, so it kept him in energy storage mode for longer. Meanwhile, the elevated insulin and elevated blood glucose were doing damage throughout Tarzan’s body.
Tarzan spent the morning feeling sluggish and thinking about food. He was supposed to be learning about the software he was going to support but he was in a bit of a mental fog. He did stir himself to ask a couple of pertinent questions, such as, “What is software?”
When lunchtime finally arrived Tarzan gratefully went to a nearby Wendy’s and secured a Dave’s Double combo, with fries and a Coke. The fat in the meal was broken down and sent along to fat cells for storage.
The sugar in the bun and the Coke was split into fructose and glucose. Some of the fructose was converted to glucose, with the rest sent to the liver and was mostly converted to fat and sent to the fat cells for storage. It was far more fructose than Tarzan’s liver was designed to handle and so some of the fat ended up deposited locally in the liver.
The starch in the bun and the fries was immediately converted to glucose and released into Tarzan’s bloodstream. The pancreas sensed the increased glucose and released insulin to deal with it. The insulin told the fat cells to store fat, the muscles and other tissues to burn glucose, and the liver to convert glucose to fat. The barrage of glucose was more than his liver was designed to handle, and so some was left behind as fat in his liver.
Tarzan’s glucose and insulin climbed much higher and took far longer to come down than had ever happened back in the jungle. It took a long time before the insulin dropped enough that his brain could get the message that it was okay to move around and to stop thinking about food.
And so it went, meal after meal, day after day.
Back in the jungle Tarzan would eat a meal, he would store the fat, then as insulin fell the fat was released and his mitochondria used it to make energy. He cycled freely back and forth between energy storage mode and energy burning mode.
Now Tarzan was spending far more time in energy storage mode—and consuming more calories than he was burning—and it was starting to show. He had added a little softness around the middle, which got a little more pronounced with each passing year.
Occasionally Tarzan would attempt to lose some weight and would sometimes succeed, for a time. He counted calories and practiced portion control. He would cut down on the sweets and soda, but he still thought about food all the time. His body chemistry was in energy storage mode for too much of the time, and though Tarzan was a man of strong will, he would eventually give in. He was no match for his hormones. He always gained the weight back, usually with a little extra.
Every year Tarzan went in for his physical, and every year his doctor checked his fasting glucose. Every year it was fine. What Tarzan didn’t know was that each year it took more insulin to achieve that result. Back in the jungle it didn’t take much insulin to keep his glucose under control. Each year in America, while eating like an American, it took a little bit more. Due to the constantly elevated insulin and the fat in his liver, Tarzan was becoming insulin resistant.
A few years on, at the yearly physical, Tarzan’s doctor pointed out a few concerning items (coincidentally, I used to dance under the name “Tarzan’s Doctor”). For one, his blood pressure was up, not super high but out of the normal range. His triglycerides were on the high side, and his HDL cholesterol was on the low side.
The doctor told Tarzan that the lab numbers and extra weight around the belly showed that he was at risk for heart disease. He told Tarzan he needed to lose some weight and gave him a pamphlet detailing what a healthy diet looks like: plenty of whole grains, fruits, vegetables, lean meats, and not much saturated fat.
What Tarzan didn’t know was that his insulin resistance had progressed to something called “metabolic syndrome.”
Now Tarzan was concerned. He resolved to start eating healthy foods. He cleaned out the cupboard and went to the grocery store to stock up. The first day of his new healthy lifestyle he had a breakfast of Kellogg’s Total 100% whole grain cereal with skim milk, along with a glass of orange juice.
As Tarzan ate this healthy meal, his body started to break it down.
The fat in the meal was sent to the fat cells for storage. The protein in the milk was used to repair and grow tissues. The sugar in the cereal was split into fructose and glucose. There was a huge load of fructose in the orange juice, most of which went to Tarzan’s liver (along with the fructose from the cereal), where much of it was converted into fat and sent to the fat cells for storage. It was far more fructose than his liver was designed to handle, and some of the fat ended up deposited in his liver. The starch in the cereal was broken down into glucose, and so stimulated the pancreas to secrete insulin to deal with it. Muscles and other tissues started burning the glucose, the liver started converting glucose to fat, and the fat cells were grabbing the fat and holding onto it. It was a much larger load of glucose than Tarzan’s liver was designed to handle and some of the fat was deposited there.
Even though the fat cells were storing more fat, Tarzan’s brain wasn’t getting the signal that his fat reserves were full because of the elevated insulin. He felt sluggish and thought about food all morning.
For his lunches, Tarzan had bought a variety of “Healthy Choice” frozen dinners. This day he had brought the chicken parmigiana. With over forty grams of carbohydrate (eleven of which was sugar), it had pretty much the same effect as his breakfast. The meal left Tarzan’s liver a little fatter and more insulin resistant than before.
For his afternoon snack, Tarzan opted for a large “Acai Super Anti-Oxidant” smoothie from Jamba Juice. To Tarzan that sounded like about the healthiest thing he had ever heard of. Tarzan didn’t realize that he was getting eighty-eight grams of sugar, more than twice as much as in a twelve ounce can of Pepsi. His liver just whimpered and raised a white flag.
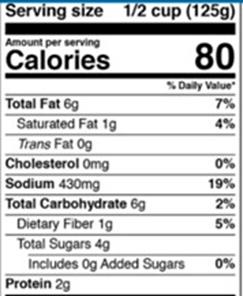
For supper, Tarzan had some whole grain pasta, with some whole grain garlic bread and a side of asparagus. The fat in the meal was sent to his fat cells for storage. The protein from the meat in the spaghetti sauce was used for tissue growth and repair. The starch in the whole grain pasta and bread turned to glucose. His blood glucose spiked and remained high for much too long, and so it was a long time before his glucose and insulin dropped low enough that he could start burning fat again.
Tarzan maintained this healthy eating pattern by scrupulously following the guidelines in the pamphlet. He had yet to learn that just because a food is advertised as healthy doesn’t mean it is.
After three months of this supposedly healthy eating, Tarzan returned to his doctor for a follow-up. He was excited to see how much his lab numbers had improved. This proved a disappointment, to both Tarzan and his doctor. There was no detectable improvement. His doctor said he must simply be eating too much and advised him to cut back on his portion sizes. Tarzan was despondent.
Though Tarzan loved America and loved being with Jane, his life was not without its dissatisfactions. In addition to feeling sluggish much of the time, he was under a great deal of stress at work. Every time he made a mistake on his TPS reports, five different bosses would come by his cubicle and let him know about it. And many of the callers to his technical support line would become inexplicably enraged. He wasn’t sleeping well. He had taken to staying up late, binging on Netflix and scrolling through his twitter feed. He would go to bed late and have difficulty falling asleep. When the alarm went off in the morning, he would hit snooze over and over and it would take a long time for him to stop feeling groggy. He had made friends in America, but he didn’t get to spend as much time with them as he would have liked. He would meet his friends for lunch or accompany Jane on a couples outing on occasion, but he missed those long hours rambling through the jungle or sitting around the fire with his buddies. Also, as Lord of the Jungle, Tarzan had felt a strong sense of purpose, something lacking in his life in America. And on top of all that he had become depressed. That had never happened in the jungle. He had experienced sadness, even grief, but never just this vague sense of despair.
Then Tarzan had an epiphany.
He remembered how happy he had been back in the jungle. He was healthy and full of energy. He wasn’t under constant stress; he had a strong sense of community and a strong sense of purpose. Leaving Jane to return to the jungle was out of the question, so Tarzan decided to try to replicate his jungle life as nearly as possible.
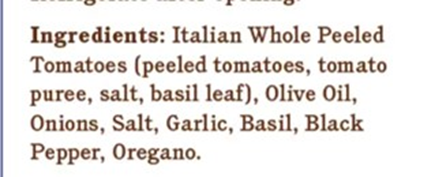
He decided he was done with diets. They had only let him down. He remembered that in the jungle he just ate real food—stuff that came out of the ground and stuff that came from animals. He resolved to eat the same way in America. Once again he cleaned out the cupboards and brought in an entirely different set of groceries.
The first morning of the new regime, Tarzan had eggs scrambled in butter, some blueberries, and a glass of whole milk. The fat in the eggs, butter, and milk was packed up and sent to the fat cells for storage. The fructose in the blueberries was mostly converted to glucose in his intestines, with the remainder sent to the liver to be converted to fat and sent to the fat cells for storage. There wasn’t a great deal of fructose (and what there was bound up with fiber and so entered his bloodstream more slowly), so his liver was able to handle it with no problem. It breathed a sigh of relief. The sugar in the milk ended up as glucose, which, along with that in the blueberries, stimulated his pancreas to secrete insulin. Since there was less glucose resulting from this meal than Tarzan had grown accustomed to, a good deal less insulin was released. But it still did its job, telling the muscles to burn the glucose, the liver to convert it to fat, and the fat cells to store the fat. Since it was a smaller glucose load, the liver was able to handle the volume with no problem.
At lunch Tarzan had a grilled chicken Caesar salad. His liver was ecstatic.
For supper Tarzan grilled a nice ribeye steak, with some green beans and broccoli on the side. He had strawberries with cream and pecans for dessert. His body broke those down in the usual ways. The fructose and glucose loads were manageable. His liver, for the first time in a long while, was able to take the rest of the evening off and put its feet up.
Tarzan continued to eat just real food, eating when hungry, and stopping when full. He didn’t realize it was happening, but his liver had been taking advantage of the lighter load and had started clearing out some of the fat. His liver was becoming more sensitive to insulin. Since his food wasn’t causing the high glucose spikes, his insulin levels were down. His other tissues were becoming more insulin sensitive.
One afternoon a few weeks later Tarzan experienced something he hadn’t felt for a long time. He found himself fidgeting and wanting to move. When break time came, he got up and went for a walk instead of checking out the responses to his latest facebook posts. Tarzan didn’t realize it, but his insulin levels were now dropping low enough for his brain to get the signal that his fat stores were full. It now knew that Tarzan was not starving and started letting him know it was okay to move and to stop eating. Tarzan’s food cravings subsided considerably.
He was feeling more energetic and started moving and exercising again. When he got home from work he no longer felt the desire to sit on the couch and reach for the remote. He could often be seen of an evening walking his monkey in the park. For the longest time exercise had been a chore and a duty; it was becoming a joy. He was gaining muscle mass and his heart and lungs were growing more efficient. And the activity and exercise helped to improve his insulin sensitivity even more.
His newfound energy spurred him to make other changes. He deleted his Twitter and Instagram accounts and made sure to turn off all screens well before bedtime. He made sure he got out in the sun every morning. He found that the local zoo was in need of an assistant to the zookeeper (not an assistant zookeeper) and applied immediately. He won the job, and the zookeeper was impressed with the rapport Tarzan had with the animals. The job change not only removed the source of much of Tarzan’s stress, but looking after the animals gave him the sense of purpose he had been lacking. He deepened his relationships with his friends, spending more time together and inviting them over for long evenings around the firepit on his patio.
Tarzan wasn’t aware of it, but because of his lowered fructose and starch intake his liver wasn’t converting nearly as much fructose and glucose to fat and so there was quite a bit less of it in his bloodstream to show up on his lab report as high triglycerides. He also didn’t know that his lowered insulin levels and increased insulin sensitivity were helping his blood pressure to normalize.
A few months later he had another follow-up with the doctor. The doctor was surprised and pleased that Tarzan had lost some weight around the belly. He was even more pleased that Tarzan’s blood pressure and lab numbers were improved. In increasing his insulin sensitivity Tarzan had reversed his metabolic syndrome. He had gone a long way toward recovering his metabolic health.
I’d like to say that Tarzan never strayed from his new path and continued to improve his metabolic health without stumbling. But that would be wrong. For one thing, the reward center in his brain never forgot those dopamine hits from his first taste of pancakes and syrup, and so was constantly prodding him to chase that dragon. And the whole world was conspiring to lead him astray. There were ads for sweets everywhere, and every social gathering featured a lot of foods that could throw him off track.
After one annual physical his lab report was so good that he decided to celebrate with a cheat meal. He went to a diner and ordered an omelet, with hash browns and biscuits and gravy. It awakened something deep in his soul. After the meal he remembered how good Dr Pepper tastes and decided to have one before going back to eating just real food. Then it occurred to Tarzan that he hadn’t had pizza in a long time, and he could have that for supper and start eating right the next day. He did so, and followed it up with a slice of apple pie and ice cream for dessert. It was a few months before Tarzan came to his senses and started eating just real food again. He had gained back some of the weight, and was feeling sluggish and tired.
Most of his setbacks were temporary. He attended a potluck with friends from church. Though he had resolved to not eat poorly at the potluck he found that when confronted with a skillet full of blackberry cobbler he was powerless to resist. He had a very small slice—it was only wafer thin—followed shortly thereafter by a much larger slice, which was followed by half a family-sized bag of Lay’s potato chips. He was back on track the next day, but paid for his excesses with a couple of days of feeling pretty crummy.
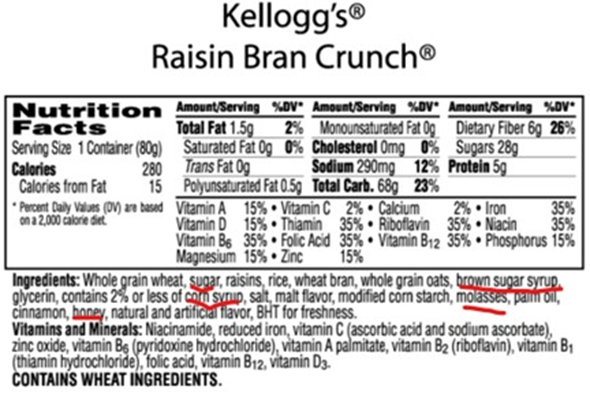
Another time he had purchased a box of Total Whole Grain Cereal, just to see how his body responded to it. He found that it spiked his blood sugar to an unwelcome extent and resolved not to include it as part of his regular diet. But he neglected to throw away the box. The next evening he came home from work and found the box on the kitchen counter. He proceeded to eat three bowls of it in rapid succession—an act he came to bitterly regret for reasons upon which I shall not elaborate.
But eventually Tarzan figured out the strategies to navigate this treacherous world. He also figured out which foods he could safely eat, and which would set him on a downward spiral. He learned strategies that would allow him to occasionally eat treats without triggering binges.
He learned to identify natural fats, and came to understand how different kinds of fats affected his metabolic health.
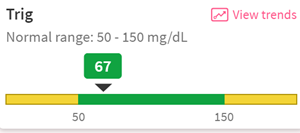
Tarzan also learned how to measure his metabolic health to ensure that he was eating an optimal diet.
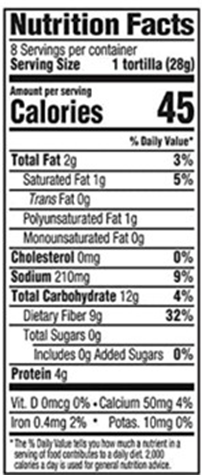
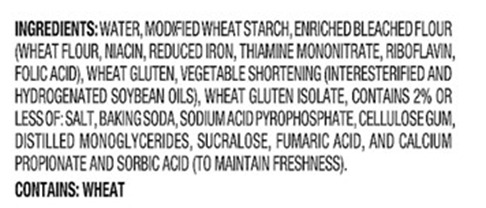
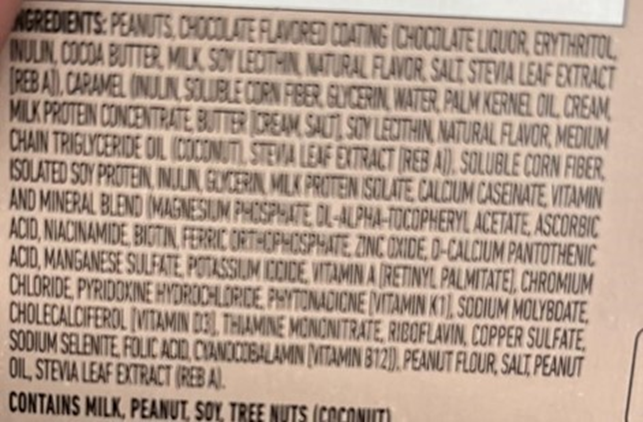
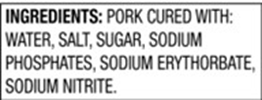
He learned to read labels on food packages so he could avoid metabolically damaging foods.
Tarzan had figured out a metabolically healthy lifestyle. Tragically, Tarzan was hit by a bus and killed shortly before his fiftieth birthday.
I’m kidding! Tarzan lived to an advanced age, dying at ninety-three in a fall while trying to rescue a neighbor’s cat from the upper branches of an oak tree. (The cat was never in any actual danger. He came down on his own when the ambulance arrived to see what all the fuss was about.)
***************
Tarzan’s story is not at all unique. Millions of people around the world have gone through the same transition, from metabolic health to metabolic dysfunction. In the nineteenth century and into the twentieth, there were countless reports from explorers, colonial doctors, missionaries, and others detailing the remarkably good health of indigenous populations while eating their traditional diets. These reports came from across Africa, Asia, Australia, and the Americas. The reports were consistent: while the populations may have suffered from infectious diseases, parasites, and trauma, they were remarkably free of diabetes, heart disease, and cancer.
This was true even of the very old.
And these people groups were eating a wide variety of traditional diets: it included the Inuit, who ate almost exclusively meat with very high levels of fat consumption and almost no carbohydrates; it included the south sea islanders who ate a diet rich in unrefined carbohydrates along with a lot of fish and coconut; it included the Masai who consumed mostly meat, milk and blood.
One thing these groups had in common was what they lacked: sugar and refined carbohydrates (e.g., flour).
But another thing these cultures had in common was that when they started incorporating sugar and flour into their diets, they started experiencing what came to be called “diseases of civilization”: diabetes, cancer, heart disease, and dementia (among others).
Sadly, most of those folks did not have the same opportunity to correct their diet and lifestyle that Tarzan had.
Foods that raise the levels of fructose, glucose and insulin in our blood contribute to all manner of chronic disease. And these problems don’t just suddenly begin to develop the moment someone is diagnosed with type II diabetes. They have been developing all along as insulin resistance morphs into metabolic syndrome and on into diabetes.
Those foods include, I am sorry to say, sweets, soft drinks, sports drinks, orange juice (and other fruit juices), fruit smoothies, and the million and one processed foods that have added sugar that we don’t even notice.
They include bread, pasta, chips, crackers, breakfast cereals (even the “healthy“ ones), and the million and one processed foods that are loaded with refined carbohydrates.
They include salad dressings, sauces and fried foods brimming with unnatural fats and oils.
I fully realize that the lists above contain many of our favorite foods. I’m not one of those people who doesn’t understand why everyone doesn’t just eat kale. I didn’t pack on an extra 120 pounds by being indifferent to cookies, bread, and pasta. The thought that I can no longer eat biscuits and gravy occasions in me an emotion not unlike grief. But these are the very foods that are making us fat and sick.
I am not saying you should never eat these foods again; rather that you might consider them treats for occasional indulgence instead of staples of your diet.
There are unicorns among us who can eat lots of these foods and retain their metabolic health (just as there are people that live into their nineties while smoking three packs a day). And there is a great deal of variation among humans, and so likely there is not one diet that fits everyone. But it is likely that anyone would benefit from reducing or eliminating processed foods.
If you would be interested in learning about the science behind Tarzan’s story, or would like to get some tips on how you can follow Tarzan’s path back to metabolic health, see the posts below. At the very end you will find links to references relating to the science discussed in the story.
Contact: Should you wish to respond to all this, or just want to tell me I said something dumb, shoot me an email at ron_harrington@icloud.com.
About me: I live near Tulsa, Oklahoma, where I am employed as an IT infrastructure engineer. I no longer dance professionally.